Peripheral arterial disease (PAD) is common in adults and affects approximately 8 to 12 million Americans over the age of 40 every year, though actual numbers are likely higher due to under or misdiagnosis. The most common type of PAD, called “lower extremity PAD,” is caused by an accumulation of plaque in the arteries of the legs, which reduces the flow of blood carrying oxygen and important nutrients to surrounding tissues.
Unfortunately, many people mistake the symptoms of peripheral arterial disease for something else, and when left untreated, PAD can lead to gangrene and amputation of the lower extremities.
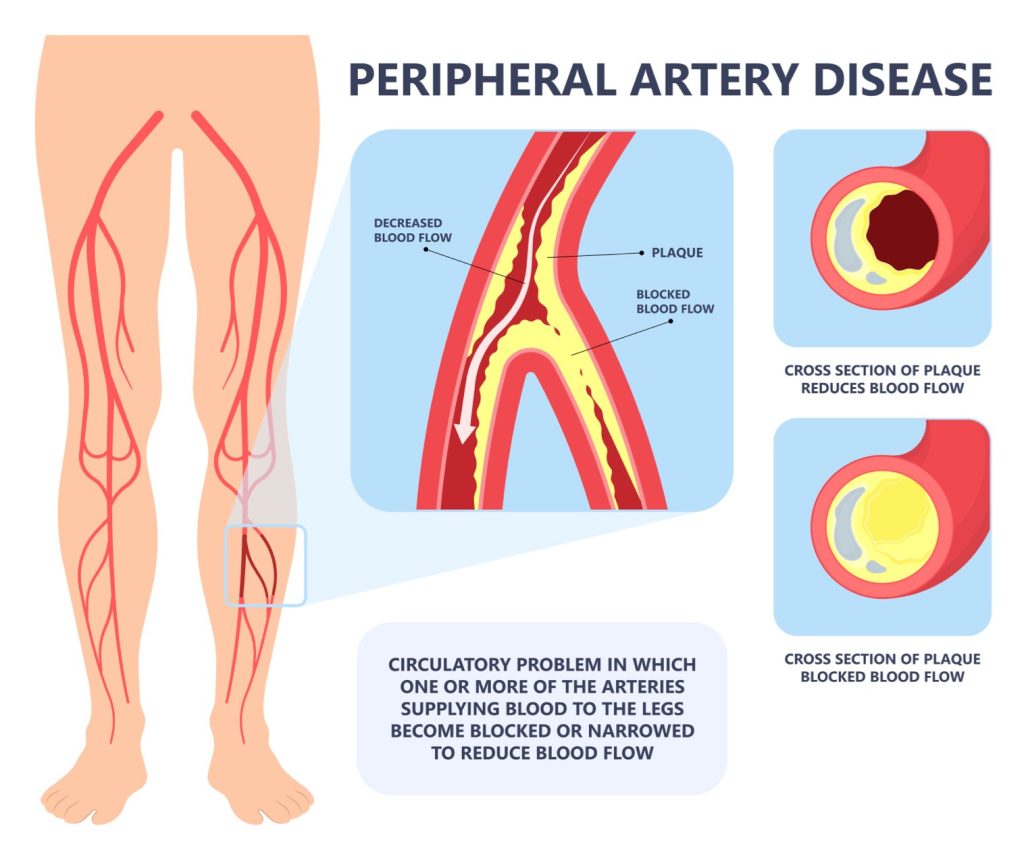
What is Peripheral Arterial Disease?
As mentioned above, peripheral arterial disease is the buildup of plaque in the arteries of your leg(s) that prevents blood from carrying oxygen and nutrients to your lower extremities. Also known as atherosclerosis, this plaque is often hard on the outside and soft on the inside. The hard shell is prone to crack, allowing platelets (blood clotting agents) to form around the plaque, further narrowing the arteries.
As blood flow is slowly cut off to the lower extremities, tissue damage can occur below the blockage, causing eventual death (gangrene) of tissue in your toes and feet. This can lead to critical limb ischemia and amputation of the affected limb.
Peripheral Arterial Disease Symptoms
Peripheral arterial disease can be overlooked or misdiagnosed because the symptoms are often varied and may be caused by other maladies. Likewise, many people with PAD attribute their symptoms to lifestyle or age-related aches and pains and forego seeing a doctor until the disease has significantly progressed.
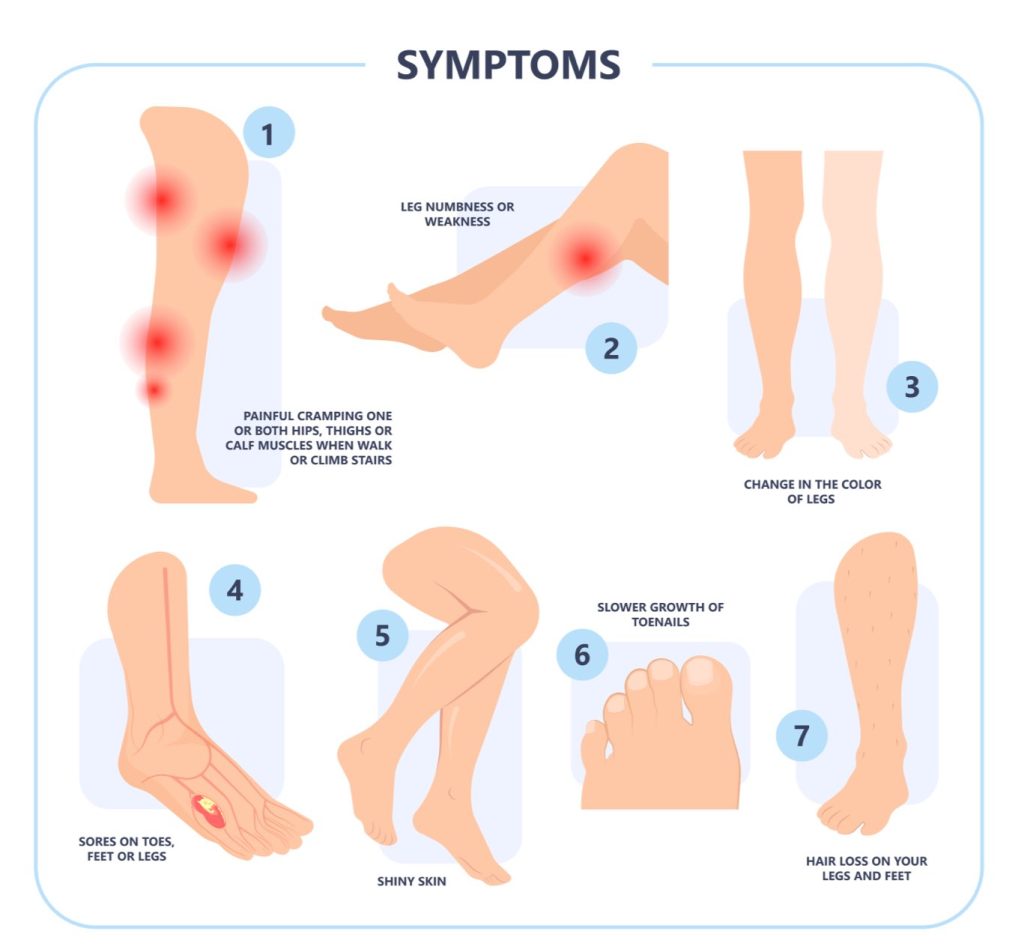
While people with PAD experience leg (calf and/or thigh) pain while walking (called claudication) that gets better with rest, others exhibit mild or no symptoms. In fact, up to 4 in 10 people with PAD have no leg pain, though claudication can also occur in the hip or buttock. As PAD progresses, pain may occur even when lying down or resting.
Other signs and symptoms of the peripheral arterial disease:
- Leg numbness or weakness (atrophy)
- Coldness of the lower leg or foot (particularly when compared to the other side)
- Painful cramping in the hip or thigh after activity or exercise
- Burning or aching pain in toes and feet (particularly while resting or lying down)
- Weak or no pulse in the legs or feet
- Shiny skin or color changes on the legs
- Hair loss and/or slower hair growth on the legs
- Slower toenail growth
- Sores or ulcers on the legs, feet, or toes
PAD Causes & Risk Factors
Peripheral arterial disease is primarily caused by atherosclerosis – the buildup of fatty, cholesterol-containing deposits (called plaques) on the artery walls of your legs and, less commonly, your arms. This buildup of plaque can reduce blood flow through arteries throughout the body, not just in the limbs, increasing the risk of developing coronary artery disease and cerebrovascular disease, which could lead to a stroke or heart attack.
While atherosclerosis is the main cause of PAD, there are less-common causes, including:
- Acute limb injury
- Changes to the muscles or ligaments in the arms and legs
- Blood vessel inflammation
- Radiation exposure
What are the risk factors for PAD?
While PAD is often first diagnosed in middle age, the prevalence of peripheral arterial disease increases with age in both men and women and is noticeably higher in people over the age of 80 and people of African American descent.
By far the biggest risk factor for developing peripheral arterial disease is tobacco use. Studies have found that tobacco use increases the risk of PAD by 400% and brings on PAD symptoms nearly 10 years earlier than non-smokers. Approximately 80% of people with peripheral arterial disease are smokers or ex-smokers.
Other PAD risk factors include:
- Diabetes
- High blood pressure
- High cholesterol
- Family history of PAD, heart disease or stroke
- Abdominal obesity
- Kidney disease (both a risk factor and consequence of PAD)
- High homocysteine levels (amino acid), which increase the risk of coronary artery disease
- Age above 60 years
Diagnosing PAD

If you’re experiencing symptoms of peripheral arterial disease, you should see a podiatrist or foot and ankle specialist right away, as PAD is easier to manage the sooner it’s diagnosed. Luckily, PAD is usually simple to diagnose with a noninvasive test called an ankle brachial index (ABI), which measures the blood pressure in your ankles and compares it to the blood pressure in your arms, both during exercise and at rest.
If your doctor wants a deeper look after the ABI, he or she may also perform additional imaging tests, such as an ultrasound, computed tomographic (CT) angiography, or magnetic resonance angiography (MRA).
Peripheral Arterial Disease Treatment
Your podiatrist or foot and ankle specialist may prescribe high blood pressure, high cholesterol, and/or diabetes medications, if necessary. While these are not cures for PAD, they treat the risk factors of PAD and help reduce the risk of heart attack and stroke. Your doctor might also prescribe an antiplatelet medication, like aspirin, or medication that eases claudication during exercise.
Peripheral Arterial Disease Self-care
One of the best ways to treat PAD is through lifestyle changes and self-care. First and foremost, it’s imperative to stop using tobacco products, if applicable. Regular exercise is also very important for treating PAD and simply walking every day is one of the best exercises for treating peripheral arterial disease.
Other lifestyle and self-care PAD treatments include:
- Eating a balanced high-fiber diet that is low in cholesterol, fat, and sodium
- Lowering stress levels (consider yoga and meditation)
- Managing high blood pressure, high cholesterol, and/or diabetes
- Practice good skin and foot care
For people with severe PAD who do not see improvement with medication and lifestyle changes, minimally invasive endovascular or surgical treatment may be required to relieve pain and improve blood flow.
If you’re experiencing symptoms of peripheral arterial disease, the sooner you start treatment, the better for your future health and overall quality of life. If you have any questions about PAD or would like to schedule an appointment with a specialist, please contact us today.