Diabetic neuropathy is one of the most common complications associated with diabetes, affecting millions of people worldwide. Up to 50% of people with diabetes have peripheral neuropathy and more than 30% have automatic neuropathy. Diabetic neuropathy occurs when prolonged high blood sugar levels damage the nerves throughout the body. The condition develops gradually and usually affects the nerves in the legs and feet, although different types of diabetic neuropathy can also impact the arms and hands.
This condition can lead to a range of symptoms, from pain and numbness to more severe complications like sexual dysfunction and issues with the autonomic nervous system.
What causes diabetic nerve damage?
Chronic high blood glucose (also called blood sugar) from uncontrolled diabetes and high triglyceride (fat) and cholesterol levels in the blood can damage nerves throughout the body. High blood sugar can also damage the walls of tiny blood vessels that supply oxygen and nutrients to nerves.

Vascular issues, like high blood pressure, and inherited factors can also contribute to poor circulation and impaired blood flow. Under these conditions, the nerves can also become injured, inflamed, or die off. Over time, symptoms worsen as more nerves are impacted.
Types of Diabetic Neuropathy & Symptoms
There are four main types of diabetic neuropathy, and symptoms can widely depending on the type of nerves affected.
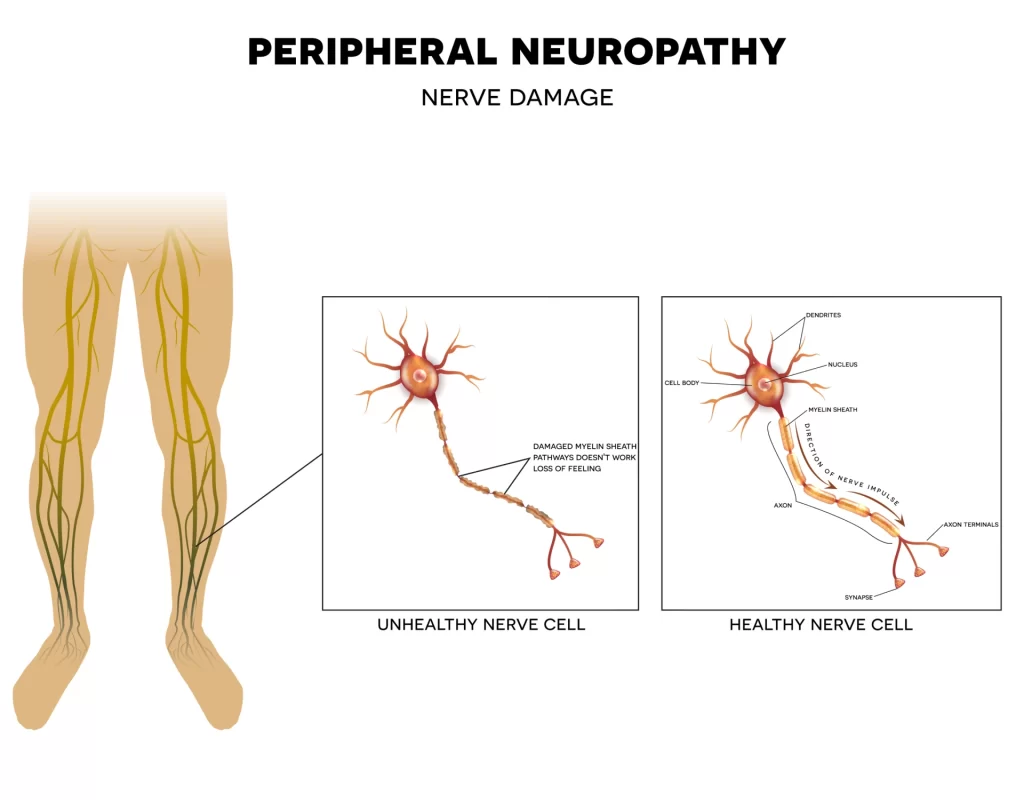
Peripheral Neuropathy
Peripheral neuropathy, also called distal symmetric peripheral neuropathy, is the most common type of diabetic neuropathy. This type usually starts in the toes and soles of the feet and causes pain or numbness in the feet or legs, followed by symptoms in the hands and arms. This pain is often described as stabbing, sharp, tingling, or burning and can be debilitating.
Common symptoms include:
- Numbness
- Tingling or burning sensations
- Cramps or sharp pains
- Muscle weakness
- Reduced ability or inability to feel temperature changes
- Extreme sensitivity to touch
- Reduced ability to feel pain leading to serious complications (ulcers, infections, bone and joint damage)
Autonomic Neuropathy
Autonomic neuropathy affects the autonomic nervous system, which controls involuntary functions like heart rate, blood pressure, sweating, digestive system, sex organs, and other autonomic functions. This can cause problems with blood pressure regulation, digestion, bladder and bowel movements, vision, and swallowing. Autonomic neuropathy can also cause sexual dysfunction for men and women, and even affect the ability to sense hypoglycemia.
Proximal Neuropathy
Also called diabetic polyradiculopathy, proximal neuropathy typically affects the legs, thighs, buttocks, and hips. Symptoms include severe pain in the affected area, difficulty getting up from a seated position, weakening of the thigh muscles, and pain in the chest or abdominal wall. Though proximal neuropathy typically affects one side of the body, it can spread to the other side.
Mononeuropathy
Mononeuropathy, or focal neuropathy, is damage to a single nerve in a leg or arm, or the torso or face. The symptoms of this type of diabetic neuropathy vary greatly depending on the affected nerve but may include partial facial paralysis, vision problems, numbness and tingling, weakness in the affected area, and pain.
Is diabetic neuropathy reversible?
Unfortunately, nerve damage caused by diabetes is generally considered irreversible. While there is currently no cure for diabetic neuropathy, early intervention to prevent permanent nerve damage can improve outcomes for people with diabetes. Managing the symptoms and preventing further progression is achievable through a combination of medical interventions, lifestyle changes, and self-care practices.
Diabetic Neuropathy Medication
While there are no medications that treat diabetic neuropathy, prescriptions such as anticonvulsants and antidepressants (such as duloxetine, pregabalin, and gabapentin) may be prescribed to help manage pain associated with diabetic neuropathy. Topical treatments like capsaicin cream can provide relief for localized pain.
Diabetic Neuropathy Self-Care
Careful management of blood sugar levels is crucial in preventing further nerve damage. Consistent monitoring and adherence to a diabetes management plan can significantly impact the progression of neuropathy and regular exercise, particularly activities that improve circulation and nerve function, such as walking, can be beneficial.
Recommended Lifestyle Changes, Footwear & Self-Care
- Work closely with a doctor to control blood sugar with diet, exercise, and medication
- The best shoes for diabetics with neuropathy are shoes with cushioned soles and toe guards to prevent injuries and trauma to numb feet
- Increase blood flow with light physical activity
- Relax inflamed nerves by soaking feet in warm (not hot) water
- Massage feet with carrier oils multiple times per day
- Take supplements like alpha lipoic acid, acetyl L-carnitine or curcumin
- Lower blood pressure through diet and medication if it is high
- Stop smoking to improve circulation
- Get 6 to 8 hours of sleep nightly
While diabetic neuropathy is generally considered irreversible, the condition does not have to prevent one from living a full life. A holistic approach, combining medications, self-care practices, and lifestyle adjustments, can significantly improve the quality of life for individuals dealing with diabetic neuropathy. When it comes to managing diabetic neuropathy, controlling its progression is key. Adhering to a comprehensive diabetes management plan that includes regular medical check-ups with diabetes specialists and a podiatrist, can help in early detection and timely intervention.