If you are experiencing prolonged pain, stiffness, and swelling in one or both feet that make walking and getting around difficult, you may be suffering from arthritis of the feet. A generalized term for a group of 100-plus diseases, “arthritis” simply means inflammation of a joint and its surrounding tissue. The causes of arthritis vary and the condition can be considered acute or chronic.
Foot Anatomy & Arthritis
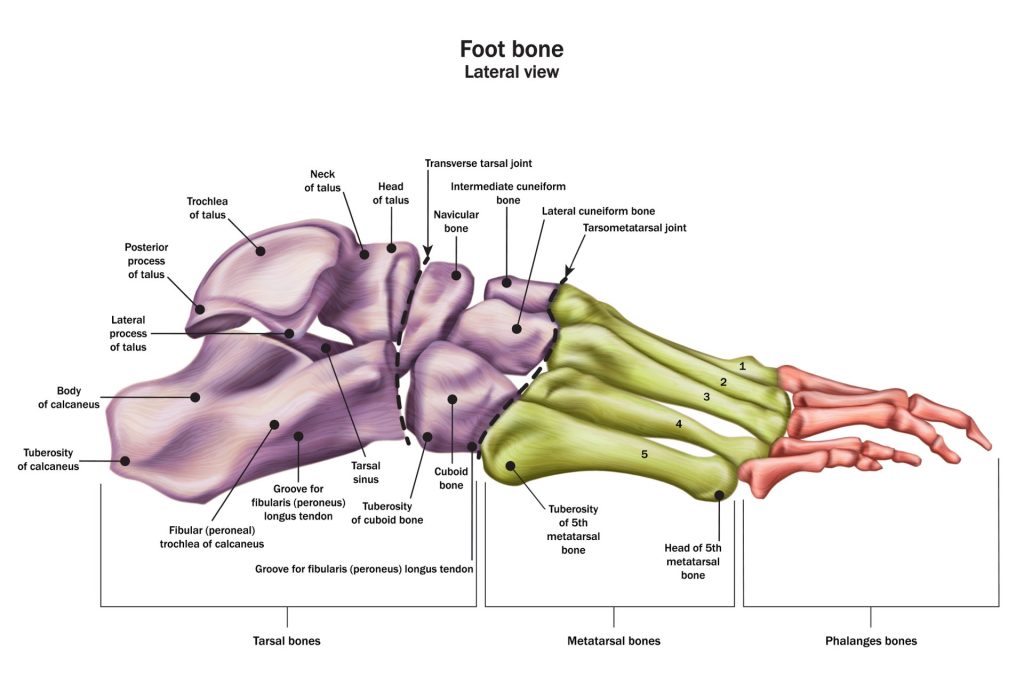
The foot is an extremely complex and somewhat delicate structure made up of 33 joints, 26 bones, and more than 100 muscles, ligaments, and tendons. Together, these structures allow you to not only bear weight but also run, jump, balance, and transfer force.
Most of the joints in the foot connect two bones. The ends of these bones are wrapped with a slippery substance called articular cartilage that allows them to glide past each other without friction or pain when you move. The joints also have a thin lining – called the synovium – that produces a fluid to further lubricate the cartilage protecting the bones. In general, arthritis of the foot occurs when these protective lubricants are damaged, making them unable to protect the bones within joints from rubbing against each other.
Types of Arthritis in Feet
While there are more than 100 types of arthritis that affect joints throughout the body, there are three main types of arthritis in feet.
Osteoarthritis of the Foot
Known as “wear and tear” arthritis, osteoarthritis occurs as cartilage is worn down with time and age. Most common in people over 50, osteoarthritis is a degenerative disease that can develop in or affect a single joint – such as a foot. As a joint’s cartilage becomes rough and frayed, it can no longer protect the bones within the joint from rubbing against each other, which can cause swelling, stiffness, and painful bone spurs (osteophytes).
Osteoarthritis of the foot is a disease that develops slowly and gets progressively worse over time. While it is most common in middle age, osteoarthritis can affect younger adults, as well.
Rheumatoid Arthritis in the Feet
Unlike osteoarthritis, which is a wear-and-tear disease, rheumatoid arthritis (RA) is an autoimmune disorder that affects the joints. Autoimmune diseases cause the immune system to attack its own tissues; in this case, RA attacks the synovium (joint lining). Also unlike osteoarthritis, rheumatoid arthritis in the feet typically affects both feet simultaneously and is often one of the first signs of RA. Over time, as the inflamed synovium continues to damage cartilage and bone, it can also affect the ligaments and tendons supporting the joint, which can cause joint deformity and serious disability.
Post-traumatic Foot Arthritis
Even if properly treated and healed, any traumatically injured joint is approximately seven times more likely to develop arthritis than an uninjured joint. This may be due to the fact that the body can shed hormones that stimulate cartilage cell death after an injury. Fractures and dislocations are the most prone to developing arthritis and post-traumatic foot arthritis can develop many years after the injury.
Other Types of Foot Arthritis
While osteoarthritis, RA, and post-traumatic arthritis are the three biggest types of foot arthritis, there are other common types of arthritis that affect the feet.

Gout
Gout is an extremely painful form of inflammatory arthritis that commonly affects the big toe joint (though it also commonly affects other toe joints, the ankle, and the knee). Known as “flares,” bouts of gout can last days or weeks and repeated flares can lead to a worse form of this type of arthritis called gouty arthritis. Gout can also go into remission for months or even years and, while there is no cure for gout, there are effective treatments to help with the symptoms.
Psoriatic Arthritis Feet
Like RA, psoriatic arthritis is an autoimmune disease that attacks the joints. Specifically, this inflammatory disease likes to strike where ligaments and tendons connect to bones. And with 33 joints in each foot, the feet present great targets for psoriatic arthritis. Most people who develop psoriatic arthritis in their feet also have psoriasis; however, it’s important to see a podiatrist if you’re experiencing dactylitis (severe digit swelling), heel pain, plantar fasciitis, bone spurs or nail changes (pits or dents).
Hallux Rigidus
The most common arthritic condition of the foot, hallux rigidus can be caused by normal wear-and-tear, a previous traumatic injury to the big toe, flatfoot, or a bunion. Hallux rigidus occurs when the cartilage around the joint at the base of the toe – called the metatarsophalangeal joint (MTP) – is damaged. As the cartilage wears away and the bones rub together, a bone spur (osteophyte) can occur, leading to stiffness, pain, and – eventually – arthritis.
If you’re suffering from the symptoms of foot arthritis, it’s important to see a podiatrist for proper diagnosis and treatment. While there is no cure for most arthritis, it can be managed with the help of a foot specialist. If you have any questions about foot arthritis or would like to talk to one of our medical professionals, please comment below or contact us today.